Clinical Trials for Active Medical Devices
Written by Luke Sy on 14th Mar. 2021. [video link]
In the webinar, Suzanne Williams, Co-founder and Principal of Mobius Medical, gave an overview of the what, why, and hows of clinical trials.
What is a Clinical Trial?
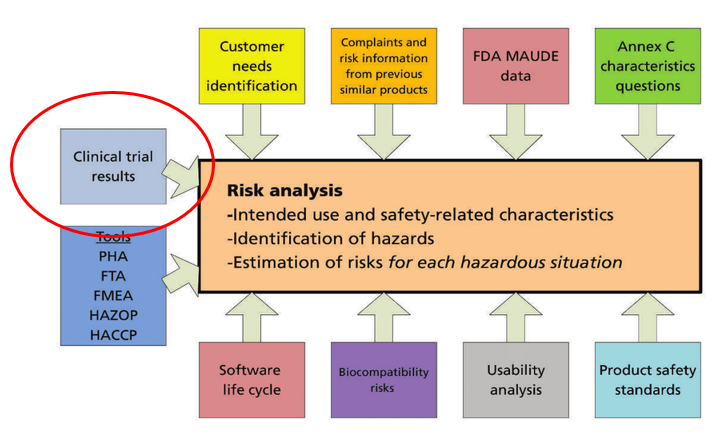
As per WHO definition, clinical trial is any research study that prospectively assigns human participants or groups of humans to one or more health-related interventions to evaluate the effects on health outcomes. From a active medical device perspective, clinical trial is important to provide clinical evidence of safety or mitigation of a particular risk associated with the device.
Clinical Trial Considerations
Type of Clinical Trial
- Pre-clinical - investigation of existing literatures leading to generating a Investigators Brochure (IB)
- Pilot - typically involves 5-15 subjects to generate safety data, and bring light the necessary device design tweaks
- Pivotal - typically involves 50-100 subjects to prove efficacy and optionally the economic benefit of the device. Usually aligned with commercial goals
- Post Approval - typically involves 100-1000 subjects, and is part of commercial roll outs whose results form the base of claims used in marketing
Developing the Clinical Investigation Plan
The factors to consider in designing a clinical investigations are listed below. The main standard for designing clinical investigations is ISO 14155.
- Device under study
- Design
- Ethical considerations
- Subject population
- Treatment and treatment allocation (e.g., comparator/benchmark, randomisation)
- Investigation variables (e.g., different standards of care between sites, learning curve)
- Concomitant medications/treatments (i.e., Hospital/state/country specific, availability, costs)
- Duration of follow up
- Statistical analysis
Law, Rules, and Guidelines that Govern Clinical Trials
In Australia, anything not listed in the Australian Register of Therapeutic Goods (ARTG) is considered as unapproved therapeutic goods. The following avenues provide for permission to import into and/or supply in Australia an unapproved therapeutic goods for use in a clinical trial: In both avenues, ethics approval by the Human Research Ethics Committee (HREC), and the final approval of the Approving Authority (i.e., institution where trial is held) are needed.
- Clinical Trial Notification (CTN) scheme -
- TGA do not evaluate any data relating to the clinical trial at the time of submission.
- Really fast turn around by TGA (2-3 days) compared to equivalent organisations in the world.
- Clinical Trial Approval (CTA) scheme.
- TGA evaluates summary information about the product including relevant, but limited, scientific data prior to the start of a trial
- Only really used for biologicals (<1% device trials use CTA)
Lastly, all research involving humans must comply with the principles set out in the following guidelines:
- National statement on ethical conduct in human research 2007 — and updates
- ICH Guideline for Good Clinical Practice / ISO 14155 (specific to devices)
Running a Clinical Trial
The subsections below describes the stakeholders, input, and output of running a clinical trial. Be aware that cost is affected by the combined factors of sample size, risk/complexity, timelines, and geography.
Stakeholders
The stakeholders of a clinical trial are the Sponsor (pays for the study), HREC (in charges from ethics point of view), Investigator (runs the study and is clinically the person in charge), Institution (location of study).
Input
- Clinical document package - includes the protocol (aka clinical investigational plan), IB, case report forms, patient informations, biomedical engineering approval
- Clinical trial agreement - includes budget, indemnity, and insurance policy
- Other Internal documents - includes Quality Management System (QMS), plans (project management and statistical analysis plan), Electronic Data Capture (EDC), visit reports
Output
- Investigator Site - source data, signed consent, medical records, lab reports, imaging
- Sponsor (manufacturer) - full dataset, statistical analysis report, clinical study report, audit reports, and trial master file